It’s been several months since the last blog-post, due to immersion in writing and editing tasks.
I’m currently working on notes for an eventual updating/revision of Muscle Energy Techniques (3rd edition)….abbreviated to MET.
A 4th edition will eventually emerge, in several years time, hence the current need for information gathering….and this post reflects some of the material I am currently working on.
Osteopathic physician Fred Mitchell Sr., was the developer of MET, then called the “muscle energy treatment.”(1958).
Mitchell wrote several papers in which he credited T.J. Ruddy, DO, as a major source of inspiration.
Ruddy (1962), a Los Angeles based practitioner who specialised in osteopathic management of head, neck and particularly eye problems, had developed a method that he had called osteopathic rhythmic resistive duction therapy – that he used to treat head and neck injury and pain.
This method involves the introduction of a series of rapid pulsating (usually patient induced) isometric contractions, against the practitioner’s resistance. A shorthand term ‘pulsed muscle energy technique’ (Pulsed-MET) is now applied to Ruddy’s method (Chaitow 2001).
In some texts Ruddy’s method is described differently, for example “In resistive duction technique, the patient’s force is constant against a rhythmic pressure applied by the osteopathic physician at a rate approximating the patient’s pulse.“
It would seem obvious that were the patient creating the rhythmic pulsation a greater degree of possible proprioceptive reeducation would be taking place, as compared with the patient resisting the operator’s pulsed efforts.
Whichever approach is used, a circulatory (lymphatic and venous) as well as a proprioceptive element occurs.
From a manual therapy perspective however, a further major benefit is the rapid normalisation of range of motion of joint restrictions when Pulsed-MET is used.
Joints as a soft-tissue problem?
The paradigm employed in use of MET or Pulsed-MET for joint restriction requires brief explanation.
Kappler & Jones observe that:
“As a [joint] barrier is engaged, increasing amounts of force are necessary and the distance decreases. The term barrier may [therefore] be misleading if it is interpreted as a wall or rigid obstacle to be overcome with a push. As the joint reaches the barrier, restraints in the form of tight muscles and fascia, serve to inhibit further motion. We are pulling against restraints rather than pushing against some anatomic structure.”
Mitchell explains further:
“Treating a joint motion restriction as if the cause were tight muscle(s) is one approach that makes possible restoration of normal joint motion. Regardless of the cause of restriction, MET treatment, based on a ‘short muscle’ paradigm, is usually completely effective in eliminating blockage, and restoring normal range of motion, even when the blockage is due to non-muscular factors”
The simplest use of Pulsed-MET involves the dysfunctional tissue or joint being held at its restriction barrier, at which time the patient (or the practitioner if the patient cannot adequately cooperate with the instructions) introduces a series of rapid (two per second) tiny efforts.
These miniature contractions toward the barrier are ideally practitioner resisted. The barest initiation of effort is called for with (to use Ruddy’s term) ‘no wobble and no bounce’.
The application of this ‘conditioning’ approach involves contractions which are ‘short, rapid and rhythmic, gradually increasing the amplitude and degree of resistance, thus conditioning the proprioceptive system by rapid movements’ (Ruddy 1962).
As mentioned, Ruddy suggests the effects are likely to include improved oxygenation, venous and lymphatic circulation through the area being treated. Furthermore, he
believed that the method influences both static and kinetic posture because of the effects on proprioceptive and interoceptive afferent pathways, so helping to maintain ‘dynamic equilibrium’ which involves ‘a balance in chemical, physical, thermal, electrical and tissue fluid homeostasis’.
The effects of Pulsed-MET might therefore include:
• proprioceptive re-education
• strengthening facilitation of the weak antagonists
• reciprocal inhibition of tense agonists
• enhanced local circulation and drainage
• re-education of movement patterns (enhanced motor control)
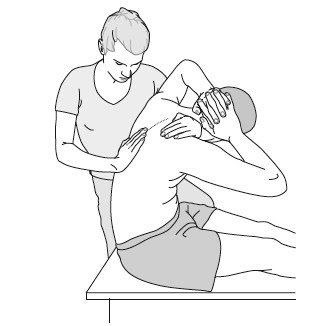
Example: Ruddy’s ‘pulsed’ MET and the erector spinae muscles (see illustration above)
To treat the erector spinae the patient should be placed on a fixed stool or chair, in a seated, slumped position, feet flat on the floor and with the head approximating the knees.
The practitioner stands behind and to the side and passes an arm across the anterior upper chest from shoulder to shoulder, while her other hand maintains a contact with the area of the back (that is being treated.
- To treat the erector spinae group a restriction barrier is engaged in which the patient is in an easy end-of-range position i.e. a combination of flexion, sidebending and rotation, with the paraspinal muscles close to their end-of-range, but not at stretch.
- The patient is coached as to the rhythm as well as the amplitude of the pulsation needed.
- This requires initiation of a series of 20 (twice per second for 10 seconds) very slight attempts to move further in the direction of the restriction barrier, pulsing against the firm and totally unyielding, resistance of the practitioner.
- After the series of mini-contractions and a brief rest, the barrier is reassessed and reengaged, and the process repeated.
- During this painless procedure the patient is rhythmically activating the antagonist muscles to those which are restricted and preventing full range of movement.
- The series of pulsing contractions tones the inhibited antagonists while reciprocally inhibiting hypertonic agonists, so increasing the range of motion.
Use of Pulsed-MET is essentially safe, and very effective .
It’s easy on the practitioner, and the patient….and it’s really difficult to understand why it is not being taught at osteopathic schools any more?
It was the foundation for MET, and deserves to be rehabilitated
REFERENCES
- Kappler RE, Jones JM. 2003 Thrust (High-Velocity/Low-Amplitude) techniques. In Ward RC (Ed) Foundations for osteopathic medicine, 2/e. Philadelphia, Lippincott, Williams & Wilkins pp852-880
- Burns D Wells M 2006 Gross Range of Motion in the Cervical Spine: The Effects of Osteopathic Muscle Energy Technique in Asymptomatic Subjects JAOA 106(3):137-142
- Mitchell FL. 1958 pelvic function. In: Barnes MW, ed. Year Book 1958: Selected
- Mitchell F Jr. 1998 Muscle Energy Manual Vol.2: MET Press, East Lansing p1 Osteopathic Papers. Carmel, Calif: Academy of Applied Osteopathy 1958:71–90.
- Ruddy T 1961 Osteopathic rhythmic resistive duction therapy. Yearbook of Academy of Applied Osteopathy 1961, Indianapolis, p 58