This post contains a summary of a presentation I will be making at the XXII Physiotherapy Conference, Madrid in March 2012, entitled:
Breathing Pattern Disorders and Lumbopelvic Pain and dysfunction : An overview.
It represents an update on my paper written in 2004, on the same theme. (Journal of Osteopathic Medicine 7(1):34-41)
For more on this topic please see my co-authored book (with Dinah Bradley PT and Chris Gilbert PhD): Multidisciplinary Approaches to Breathing Pattern Disorders. (Elsevier 2002)
Also, the newly published, coedited book (with Ruth Lovegrove PhD): Chronic Pelvic Pain and Dysfunction: Practical Physical Medicine.
A second presentation at the Madrid conference will cover a review of indirect manual treatment methods for the lumbopelvic region, and will be posted on this site, in the next few months.
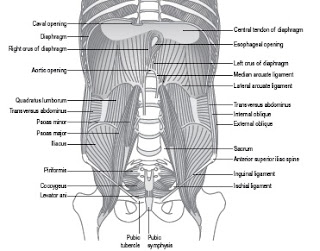
The Figure above represents the myofascial ‘inner stocking’ (or envelope) that involves a prevertebral and intrapelvic myofascial web of support. Among the key structural features of note are the multiple direct myofascial connections between the pelvic floor and the diaphragm.
Reproduced from Key (2010) J. Bodyw. Mov. Ther. 14, 299–301 – with thanks.
Summary
Breathing pattern disorders (BPD) – the most extreme of which is hyperventilation – are surprisingly common in the general population, but more so in women. Despite decades of research BPDs, together with a range of the resulting pathophysiological biochemical, psychological and biomechanical effects, remain commonly under-recognized by health care professionals as contributing to pain, fatigue and dysfunction in general and lumbopelvic pain and dysfunction, in particular. These notes focus mainly on one aspect of BPDs potentially negative influence – the contribution towards the evolution, aggravation and maintenance of lumbopelvic pain and dysfunction.
There is also recognition that pain and dysfunction contribute significantly to altered breathing patterns, so helping to create a reciprocally negative series of adaptations in which pain alters respiration, which in turn amplifies pain.
Definitions
Breathing Pattern Disorder (BPD) – also known as Dysfunctional breathing [DB] – is defined as chronic or recurrent changes in the breathing pattern, contributing to respiratory and nonrespiratory complaints. (Thomas et al 2003). Symptoms of BPD include dyspnoea with normal lung function, chest tightness, chest (and other musculoskeletal) pain, deep sighing, exercise induced breathlessness, frequent yawning and hyperventilation. (de Groot 2011)
Breathing Pattern Disorder (BPD) – also known as Dysfunctional breathing [DB] – is defined as chronic or recurrent changes in the breathing pattern, contributing to respiratory and nonrespiratory complaints. (Thomas et al 2003). Symptoms of BPD include dyspnoea with normal lung function, chest tightness, chest (and other musculoskeletal) pain, deep sighing, exercise induced breathlessness, frequent yawning and hyperventilation. (de Groot 2011)
Hyperventilation is the state in which breathing occurs in excess of metabolic requirements, leading to an acute reduction in partial pressure of carbon-dioxide (PaCO2) and a prdictable set of physiologic changes. (Lewis 1959, de Groot 2011)
Hypocapnia: Deficiency of Carbon dioxide (CO2) in the blood resulting from over-breathing/hyperventilation (HVS), resulting in increased pH, respiratory alkalosis (Naschitz et al 2006)
Respiratory alkalosis: This involves a rise in pH of the blood, from its normal levels of ~7.4 due to excessive CO2 exhalation during rapid breathing. An immediate effect is smooth muscle constriction, narrowing of blood vessels, the gut etc, as well as reduced pain threshold and feelings of anxiety, apprehension.
Respiratory alkalosis leads to decreased levels of serum calcium ions (Ca2+) despite a normal calcium level, due to a shift of Ca2+ from the blood to albumin which has become more negative in the alkalotic state. Hypocalcemia then leads to hyperirritability of nerves – evidenced by Chvostek’s sign (ipsilateral twitch of nose and lips when facial nerve tapped at angle of jaw – an early sign of tetany) (Goljan 2007)
Yee (2010) reports that: “All acid-base disturbances—respiratory acidosis, respiratory alkalosis, metabolic acidosis, and metabolic alkalosis—have the potential for producing neurologic manifestations”
Bohr effect: In an alkaline environment – such as respiratory alkalosis – haemoglobin releases oxygen less efficiently, leading to hypoxia. (Jensen 2004)
Hypoxia: Reduction of oxygen oxygen (O2) supply to tissue, below physiological levels.
Etiological and maintaining factors of BPD include:
· Psychological – for example anxiety (Han et al 1996, Nardi et al 2001)
· Biochemical – for example increased levels of progesterone (Ott et al 2006), or altered pH as in acidosis during pregnancy(Jensen et al 2008), or in other states of acidosis (Kellum 2007)
· Habit – “Neurological considerations leave little doubt that habitually unstable breathing is the prime cause of symptoms” (Lum 1984), or conditioning (van den Burgh et al 1997)
· During aerobic exercise (Hammo et al 1999)
· Nixon & Andrews (1996) suggest that deconditioned individuals utilize anaerobic glycolysis to generate, energy, resulting in relative lowering of pH, and, consequent homeostatic hyperventilation. In effect, lower pH – due to deconditioning – would trigger, hyperventilation, which would further encourage, deconditioning.
Epidemiology
In the USA as many as 10% of patients in general internal medicine practices are reported to have HVS as their primary diagnosis. (Lum 1987, Newton 2005) however BPD appears to be far more prevalent (Thomas et al 2005).
Katon & Walker (1998) noted that patients with the commonest physical symptoms (e.g., abdominal pain, chest pain, headache, back pain), are responsible for half of all primary care visits (USA), and yet only 10%–15% of these are found to be caused by organic illness. All these symptoms are well recognised as capable of being the result of BPD.
De Groot (2011) notes that the extreme of BPDs, hyperventilation syndrome (HVS), is common in adults at between 6% and 10% in different studies, and that is more prevalent in women (14%) than in men (2%).
Special populations, symptoms and BPD
· Perri and Holford (2004) reported that a convenience sample of 111 patients, attending a chiropractic pain clinic were evaluated for links between their health, pain histories and faulty breathing (criteria included evidence of obvious paradoxical –non-diaphragmatic- breathing, or a tendency to raise the upper chest to initiate inhalation). 56.4% demonstrated faulty breathing on relaxed inhalation, increasing to 75% when taking a deep breath. 87% reported a history of various musculoskeletal pain problems. Based on this self-selected population, they observe that: “Chances are 3 in 4 that new patients seen today will have faulty breathing patterns.”
· Cimino et al (2000) found that breathing rates accelerate as progesterone levels rise during the luteal phase of the menstrual cycle. This is accompanied by a simultaneous reduction in pain thresholds, suggesting that respiratory changes are at least partially influential in increased pain perception.
· In a study by Dunnett et al (2007) it was noted that several participants “changed” a diagnosis of fibromyalgia during the course of a menstrual cycle, fulfilling the diagnostic criteria during the menstrual or luteal phase, but never during the follicular phase.
· Phasic menstrual cycle changes observed in resting minute ventilation and arterial PCO(2) may be due, at least in part, to the stimulatory effects of progesterone. (Slatkovska et al 2006)
· Premenstrual symptoms (PMS) may be caused directly by hyperventilation (HVS). “It has been known for more than 100 years that women hyperventilate during the second half of the menstrual cycle. Symptoms of chronic HVS are remarkably similar to the symptoms observed in some women with PMS.… In women with PMS the sensitivity of the respiratory center to CO2 is increased more than normal by progesterone, or some other secretory product of the corpus luteum, resulting in pronounced hyperventilation.” (Ott et al 2006)
· Human pregnancy is characterized by significant increased tendency to hyperventilation largely associated, with increased circulating female sex hormone concentrations. (Jensen et al 2008)
· Baranes et al (2005) lists myalgia, back pain and muscle cramps, as common symptoms associated with overbreathing in children – with the age of onset most commonly between ages 13 and 16.
Painand BPD
· Schleifer et al (2002) outline the way in which pain may be amplified due to BPD. They explain that overbreathing results in a drop in arterial CO2, caused by ventilation that exceeds metabolic demands for O2, with a consequent rise in blood pH (i.e., respiratory alkalosis). The inevitable resulting disruption in acid-base equilibrium triggers a series of changes that increase muscle tension, induce muscle spasm, amplify the responses to catecholamines, producing muscle ischemia and hypoxia. Additionally the shift from a diaphragmatic to a thoracic breathing pattern imposes a range of biomechanical stresses.
· Terekhin and Forster (2006) have used functional magnetic resonance imaging (fMRI) involving blood-oxygen-level-dependent (BOLD) contrast, to examine ways in which the results of over-breathing impact directly on pain mechanisms. They note that this type of scan maps neural activity in the brain or spinal cord by imaging the change in blood flow (hemodynamic response) related to energy use by brain cells. Hypocapnia (reduced carbon dioxide in the blood), usually resulting from deep or rapid breathing such as hyperventilation (HVS) provides various, influences on the BOLD indicating that it may differentially affect the processing of pain input and motor tasks. “The subtle disturbances of breathing which contribute to hypocapnia should, be considered for functional brain imaging studies, especially, those examining the nociceptive system. The, decrease in BOLD signal by up to 7%, in all regions of the brain cortex, indicates a wide spread vasoconstriction in the gray matter as an acute reaction to the hypocapnia.”
· Studies also indicate that the vasoconstrictory effect of over-breathing, and resulting hypocapnia, leads to cerebral ischemia, while also increasing the affinity, of hemoglobin for oxygen due to alkalosis (Bohr effect), decreasing oxygen release into the tissue (Clausen et al 2004). The altered neuronal excitability and potentially affects both pain perception, as well as motor control.
· Diatchencko et al (2006) observed that back pain (as well as chronic neck pain) displays all the characteristics of central sensitization (Flor 2003), and that associated pain processing changes in such disorders are affected by breathing patterns.
· Individuals with back pain tend to brace their superficial abdominal muscles and diaphragm as well as having poor core muscle activation. This negatively influences normal diaphragm function, inhibiting abdominal breathing and encouraging an upper chest pattern. (Radebold et al 2001, O’Sullivan & Beales 2007)
BPD, stability, instability and the nervous system
According to Panjabi (1992) three subsystems work together to maintain spinal stability:
1. The central nervous subsystem (control): sensory receptors in the spinal structures, their central connections, and cortical and subcortical control centers
2. The osteoligamentous subsystem (passive):vertebrae, intervertebral discs, ligaments, zygapophyseal joints, and passive components of the associated musculotendinous structures
3. The muscle subsystem (active):musculotendinous units attached to, or influencing, the spinal column
These subsystems are interdependent, working together to maintain spinal stability and intervertebral motion.
There is a great deal of evidence pointing to ways in which altered breathing patterns are capable of negatively influencing both the central nervous and the active muscle subsystems, thereby contributing to the evolution or maintenance of non-pathological lumbopelvic pain and dysfunction.
· Paillard (2012) reported that hyperventilation, decreases CO2 level and increases pH in body fluids and tissues and that this provokes vascular changes, possibly responsible, for augmented postural sway (Sakellari & Bronstein (1997).
· Postural and motor control impairments have been reported extensively in chronic LBP-patients involving mal-coordination of postural and respiratory functions as well as trunk muscles. [Hodges and Mosely 2003, O’Sullivan 2005)
· Janssens et al (2010) have demonstrated that inspiratory muscles fatigue (IMF) results in “a rigid proprioceptive postural control strategy, rather than the normal “multisegmental” control, which is similar to people with LBP. This results in decreased postural stability. These results suggest that IMF might be a factor in the high recurrence rate of LBP.” Janssens et al also note that in the case of inspiratory muscle fatigue, proprioceptive input from the lower back becomes less reliable, disturbing sensory integration and thereby postural control. Overall it appears that BPD/hyperventilation affects the interoceptive sensory and motor systems of the postural control mechanism.
· Hodges et al 2005 observed that the diaphragm contributes to spinal stability in healthy subjects by adding to intra-abdominal pressure and therefore enhanced spinal stiffness. This observation built on earlier studies that indicated that the diaphragm is able to perform the dual tasks of offering trunk stability, as well as performing respiratory tasks, when trunk stability is challenged (Hodges et al 2002) – but not when sustained over-breathing is a feature. They found that after approximately 60 seconds of over-breathing, both postural (tonic) and phasic functions of the diaphragm and transversus abdominis were reduced or absent.
· Findings by Hodges et al (2001) suggest that “the stability of the spine may be compromised in situations in which respiratory demand is increased, such as exercise and respiratory disease. …..During strenuous exercise, when the physical stresses to the spine are greater, the physiological vulnerability of the spine to injury is likely to be increased”.
· This supports McGill’s (1995) study that reported that reduced spinal support is noted during a combined load challenge to the low back during breathing
challenge (e.g. digging or clearing snow).
challenge (e.g. digging or clearing snow).
· O’Sullivan & Beales (2007 have demonstrated that SI joint pain and dysfunction, are frequently associated with aberrant pelvic floor and diaphragm behaviour, and that a program that enhances motor control via rehabilitation of pelvic floor control, and a more functional respiratory pattern, improves both pain and disability
· Roussel et al (2009) have reported that more than half of patients with chronic non-specific low back pain exhibit altered breathing patterns during performances in which the trunk-stability muscles are challenged.
BPD, pelvic pain and postural considerations
The pelvic floor and the respiratory diaphragm are, structurally and functionally bound together by fascial, and muscular connections. (Lee et al 2008).
Gibbons (2001) has described the anatomical link between the diaphragm, psoas and, the pelvic floor: ‘The diaphragm’s medial arcuate ligament, is a tendinous arch in the fascia of the psoas, major. Distally the psoas fascia is continuous with the pelvic floor fascia, especially the pubococcygeus’. .
Jones (2001) has summarized the integrated structural and functional thoraco-pelvic unit as follows: “The pelvic floor muscles are part of a multi-structural unit forming the bottom of a lumbopelvic cylinder with the respiratory diaphragm forming its top and transversus abdominis the sides. The spinal column is part of this cylinder and runs through the middle, supported posteriorly by segmental, attachments of lumbar multifidus and anteriorly by segmental attachments of psoas to the abdominal muscles.”
With psoas fibres (and those of QL) merging with the diaphragm, and the pelvic floor, any degree of, inappropriate stiffness or weakness in any these muscles is likely, to impact on the ability of either of the diaphragms to function normally – compromising spinal stability.
There appears to be a clear connection between respiration and pelvic floor function as well as SIJ stability, an observation that applies particularly in women. (Hodges et al 2007)
Having analysed data from over 38,000 telephone interviews, Smith et al (2006) reported that middle-aged and older women had higher odds of having back pain when they experienced breathing difficulties, and that disorders of continence and respiration were strongly related to frequent back pain, possibly explained by physiological limitations of coordination of postural, respiratory and continence functions of trunk. They note that if pelvic floor muscles are dysfunctional, spinal support may be compromised, increasing external oblique muscle activity, overcoming pelvic floor muscle activity and possibly resulting in incontinence.
Haugstad et al (2006) observed that women with chronic pelvic pain “typically displayed upper chest breathing patterns, with almost no movement of the thorax or the abdominal area”. They also confirmed “a characteristic pattern of standing, sitting, and walking, …..lack of coordination and irregular high costal respiration”… and that “the highest density, and the highest degree of elastic stiffness [was] found in the iliopsoas muscles”.
Recognising and diagnosing BPD (Courtney et al 2009, van Dixhoorn & Duivenvoorden 1985)
- · Restlessness (type A, “neurotic”)
- · ‘Air hunger’
- · Frequent sighing
- · Rapid swallowing rate
- · Poor breath-holding times
- · Poor lateral expansion of lower thorax on inhalation
- · Rise of shoulders on inhalation
- · Visible “cord-like” sternomastoid muscles
- · Rapid breathing rate
- · Obvious paradoxical breathing
- · Positive Nijmegen Test score (23 or higher)
- · Low end-tidal CO2 levels on capnography assessment (below 35mmHg)
- · Reports of a cluster of symptoms such as fatigue, pain (particularly chest, back and neck), anxiety, ‘brain-fog’, irritable bowel or bladder, paresthesia, cold extremities (Chaitow et al 2002)
Rehabilitation
· A randomized controlled study suggested that patients with moderate chronic low back pain of an average of one-year duration, improved significantly (in both pain and functional symptoms) after either breathing rehabilitation or physical therapy for 8 weeks. (Mehling et al 2005)
· Diaphragmatic breathing, progressive muscle relaxation, exercise, self-visualization, and self-hypnosis have been shown to be effective in reducing both stress and pain perception. (Whitmore 2002)
· Chronic pelvic pain associated with chronic prostatitis, involving nonbacterial urinary difficulties, has been shown, in a study at Stanford University School of Medicine, to be capable of being effectively treated using trigger point deactivation, together with relaxation and breathing reeducation techniques. (Anderson et al 2005)
· Holloway & West (2007) report that breathing rehabilitation (Papworth Method), as part of a randomized controlled trial, involving a sequence of integrated breathing and relaxation exercises focused on BPD (including hyperventilation), led to a clinically relevant improvement in quality of life.
· Musnick (2008) has outlined a protocol that places the role of breathing rehabilitation into context, when managing musculoskeletal pain:
1. Reduce the synergistic inputs to the pain process (i.e. modify adaptive demands)
2. Deactivate trigger (or tender) points
3. Remove noxious input from scars
4. Enhance spinal and general joint functionality
5. Improve muscle recruitment, strength, flexibility
6. Pay attention to exacerbating factors in diet, lifestyle and habits (sleep, exercise, posture, balance, breathing)
7. Consider emotional/psychological factors
Conclusion
Breathing pattern disorders (BPD) can contribute to, exacerbate, and help maintain, a variety of symptoms, including lumbopelvic pain and dysfunction.
BPDs are relatively easy to recognise and diagnose, and can commonly be improved or normalised by means of a combination of rehabilitation exercises and manual therapy.
REFERENCES
Anderson RU, et al. Integration of myofascial trigger point release and paradoxical relaxation training treatment of chronic pelvic pain in men. J Urol. 2005;174:155-160
Baranes T, Rossignol B, Stheneur C, Bidat E. [Hyperventilation syndrome in children]. Arch Pediatr 2005;12:1742–7.
Cimino R, et al. Does the ovarian cycle influence the pressure-pain threshold of the masticatory muscles in symptom-free women? J Orofac Pain. 2000;14:105-111
Clausen T Scharf A Menzel M et al 2004 Influence of moderate and profound hyperventilation on cerebral, blood flow, oxygenation and metabolism, Brain Res. 1019(1–2):113–123.
Courtney R Cohen M Reece J 2009 Comparison of the Manual Assessment of Respiratory Motion (MARM) and the Hi Lo Breathing Assessment in determining a simulated breathing pattern. International Journal of Osteopathic Medicine 12:86–91
de Groot EP 2011 Breathing abnormalities in children with breathlessness. Respiratory Reviews 12 (2011) 83–87
Diatchencko L., Nackley, A. G., Slade, G. D., Fillingim, R. B. Maixner,W. (2006). Idiopathic pain disorders: Pathways of vulnerability. Pain, 123(3), 226–230
Dunnett A, et al. The diagnosis of fibromyalgia in women may be influenced by menstrual cycle phase. Journal of Bodywork and Movement Therapies. 2007;11: 99-105
Flor, H. (2003). Cortical reorganisation and chronic pain: Implications for rehabilitation. Journal of Rehabilitation Medicine, 41(Suppl), 66–72.
Gibbons, S.G.T., 2001. The model of, psoas major stability function., In: Proceedings of 1st International, Conference on Movement, Dysfunction, Sept 21–23, Edinburgh, Scotland
Gibbons, S.G.T., 2001. The model of, psoas major stability function., In: Proceedings of 1st International, Conference on Movement, Dysfunction, Sept 21–23, Edinburgh, Scotland
Goljan, EF. Rapid Review Pathology. Mosby, Elsevier, 2007; pp. 504,
Hammo A-H et al 1999 Exercise-induced hyperventilation: a pseudo-asthma syndrome, Ann Allergy Asthma Immunol 82:574-578
Han J et al 1996 Influence of breathing therapy on complaints, anxiety and breathing pattern in patients with hyperventilation syndrome and anxiety disorders. J Psychosom Res. 41:481-493
Haugstad G Haugstad T Kirste U 2006 Posture, movement patterns, and body awareness in women with chronic pelvic pain. J Psychosom Res. 61(5):637-644
Hodges P Heijnen I Gandevia S 2001 Postural activity of the diaphragm is reduced in humans, when respiratory demand increases, Journal of Physiology 537(3):999–1008
Hodges PW, Gurfinkel VS, Brumagne S et al 2002 Coexistence of stability and mobility in postural control: evidence from postural compensation for respiration. Exp Brain Res 144:293–302.
Hodges PW, Moseley GL (2003) Pain and motor control of the lumbopelvic region: effect and possible mechanisms. J Electromyogr Kinesiol 13:361–370
Hodges PW, Eriksson AE, Shirley D et al (2005) Intra-abdominal, pressure increases stiffness of the lumbar spine. J Biomech, 38:1873–1880
Hodges, P.W., Cholewicki, J., 2007. Functional control of the spine. In: Vleeming, A., Mooney, V., Stoeckart, R. (Eds.), Movement, Stability & Lumbopelvic Pain. Elsevier, Edinburgh (Chapter 33).
Hodges PW, et al. 2007 Postural and respiratory functions of the pelvic floor muscles. Neurourol Urodyn. 26 :362-371
Holloway EA, West RJ. Integrated breathing and relaxation training (the Papworth
method) for adults with asthma in primary care: a randomised controlled, trial. Thorax 2007;62:1039–42.
Janssens L Brumagne S Polspoel K et al 2010 The effect of inspiratory muscles fatigue on postural control in people with and without recurrent low back pain Spine, 35 (10):1088-1094.
Jensen D Duffinc J , Yuk-Miu Lam Y-M et al 2008 Physiological mechanisms of hyperventilation during human pregnancy, Respiratory Physiology & Neurobiology 161:76–86
Jensen F 2004 Red blood cell pH, the Bohr effect, and other oxygenation-linked phenomena in blood O2 and CO2 transport Acta Physiologica Scandinavica 182(3):215-227
Jones, R., 2001. Pelvic floor muscle, rehabilitation. Urol. News 5 (5), 2–4
Katon W Walker E. J 1998 Medically unexplained symptoms in primary care. Clin Psychiatry.59 (Suppl 20):15-21
Kellum J 2007 Disorders of acid-base balance Crit Care Med. 35(11):2630-2636
Lee D Lee LJ McLaughlin L 2008 Stability, continence and breathing:, The role of fascia following pregnancy, and delivery. J. Bodyw. Mov. Ther., 12, 333–348.
Lewis BI 1959 Hyperventilation syndrome: a clinical and physiological evaluation. Calif Med. 91:121–126.
Lum L 1984 Editorial: Hyperventilation and anxiety states. J R Soc Med. January 1-4
Lum L. 1987 Hyperventilation syndromes in medicine and psychiatry: a review. J. R Soc Med. 80:229-231.,
McGill S Sharratt M Seguin J 1995 Loads on spinal tissues during simultaneous lifting and ventilatory challenge. 38(9): 1772–1792.
McGill SM. Low back exercises: prescription for the healthy back and when recovering frolTl injury. In: Resources Manual for Guidelines for Exercise Testing and Prescription. 3rd ed. Indianapolis, Ind:
American College of Sports Medicine. Baltimore: Williams and Wilkins; 1998.
Mehling W, et al. Randomized, controlled trial of breath therapy for patients with chronic low-back pain. Altern Ther Health Med. 2005;11:44-52
Musnick D 2008 Pain sensitization and chronic musculoskeletal pain. 15th International Functional Medicine Symposium, Carlsbad CA May 22-25 2008
Nardi A et al 2001 Hyperventilation challenge test in panic disorder and depression with panic attacks. Psychiatry Research105(1-2):57-65
Naschitz JE, et al.2006 Patterns of hypocapnia on tilt in patients with fibromyalgia, chronic fatigue syndrome, nonspecific dizziness, and neurally mediated syncope. Am J Med Sci. 331:295-303
Newell, R., 2005. Anatomy of the, post-laryngeal airways, lungs and, diaphragm. Surgery 23 (11), 393–397
Newton EJ. 2007 Hyperventilation Syndrome. September 26, 2005. Available online at: http://www.emedicine.com/emerg/topic270.htm. Accessed: December 22, 2007.,
Nixon P Andrews J 1996. A study of, anaerobic threshold in chronic fatigue, syndrome (CFS). Biol. Psychol., 43(3):264
O’Sullivan P (2005) Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism. Man Ther 10:242–255
O’Sullivan P Beale D 2007 Changes in pelvic floor and diaphragm kinematics and respiratory patterns in subjects with sacroiliac joint pain following a motor learning intervention Manual Therapy 12:209–218
Ott H et al 2006 Symptoms of premenstrual syndrome may be caused by hyperventilation Fertility and Sterility 86(4):1001.e17-1001.e19
Paillard T 2012 Effects of general and local fatigue on postural control. Neuroscience and Biobehavioral Reviews 36 (2012) 162–176
Panjabi M. The stabilizing system of the spine. Part 1. Function,
dysfunction, adaptation, and enhancement. J Spinal Disorders. 1992;
5:383-389.
Perri M, Halford E. 2004 Pain and faulty breathing: a pilot
Study Journal of Bodywork and Movement Therapies. 8:237-312
Pool-Goudzwaard, A., Slieker ten Hove, M.C et al., 2005. Relations between pregnancy-related low back pain, pelvic floor activity and pelvic floor dysfunction. International Urogynecology Journal and Pelvic Floor Dysfunction 16 (6), 468–474.
Radebold A Cholewicki J Polzhofer B et al 2001., Impaired Postural control of the lumbar spine is associated with delayed muscle response times in patients with chronic idiopathic low back pain. Spine 26(7):724–730
Roussel N Nijs J Truijen S,2009 Altered breathing patterns during lumbopelvic motor control, tests in chronic low back pain: a case–control study Eur Spine J18:1066–1073
Smith M, et al. 2007 Postural response of the pelvic floor and abdominal muscles in women with and without incontinence. Neurourol Urodyn. 26: 377-385.
Sakellari V Bronstein A Corna S. et al 1997., The effects of hyperventilation on postural control mechanisms. Brain 120, 1659–1673.
Schleifer LM, Ley R, Spalding TW. 2002 A hyperventilation theory of job stress and, musculoskeletal disorders Am J Ind Med. 41(5):420-32.,.
Slatkovska L, et al.2006 Phasic menstrual cycle effects on the control of breathing in healthy women Respir Physiol Neurobiol. 154:379-388
Terekhin P Forster C 2006 Hypocapnia related changes in pain-induced brain, activation as measured by functional MRI . Neuroscience Letters 400:110–114
Thomas M, et al. 2005 The prevalence of dysfunctional breathing in adults in the community with and without asthma. Prim Care Respir J. 14:78-82
Thomas M, McKinley RK, Freeman E, Foy C, Prodger P, Price D. Breathing retraining for dysfunctional breathing in asthma: a randomised controlled trial. Thorax 58:110–115.
Van Dixhoorn J Duivenvoorden H 1985 Efficacy of Nijmegen Questionnaire in recognition of the hyperventilation syndrome Psychosom Res. 29:199-206
Van den Bergh O et al 1997 Learning to have psychosomatic complaints: Conditioning of respiratory and somatic complaints in psychosomatic patients. Psychosom Med. :13-23
Whitmore K. Complementary and alternative therapies as treatment approaches for interstitial cystitis. Rev Urol. 2002;4(Suppl 1):S28 -S35
Yee A Rabinstein A 2010 Neurologic Presentations of Acute Metabolic Disorders. Neurol Clin. 28:1–16