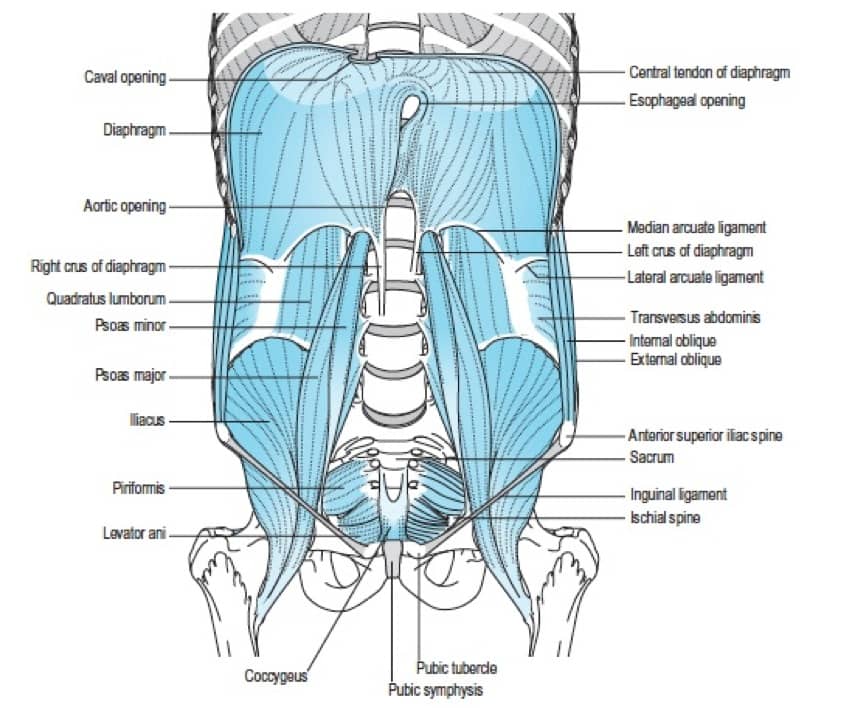
Leaving aside the profound effects of breathing pattern disorders on emotion and general health – individuals with poor posture (Lewit 1980), scapular dyskinesis (Clifton-Smith 2011), low back pain (Roussel et al 2007), neck pain (Kapreli et al 2009) and TMJ pain (Hruska 1997) – have all been shown to exhibit signs of faulty breathing mechanics, where the accessory respiratory muscles dominate over lower thorax and abdominal motion.
McLaughlin et al (2011) has demonstrated a connection between neck pain and poor respiratory chemistry that improved, together with reduced pain levels, following a program to address breathing dysfunctions alongside manual therapy to address thoracic cage mobility.
ALSO:
- Reduced spinal support is observed during combined load challenge to the low back and during breathing challenge (e.g., digging) (McGill et al 1995)
- After ± 60 seconds of over-breathing, both postural (tonic) and phasic functions of the diaphragm and transversus abdominis are reduced or absent (Hodges et al 2000)
Breathing retraining is not difficult – nor does it need to be time consuming
….and it is usually very successful in rehabilitating function and reducing or removing a huge variety of symptoms.
…and the key to the changes lies in learning how to exhale, because without effective exhalation, inhalation can never be optimal.
For many years I have taught pursed lip breathing methods – and advise two sessions daily lasting 4 to 5 minutes – comprising 30 cycles on inhalation/exhalation with emphasis on the latter being slow and complete (i.e. a pranayama yoga pattern)
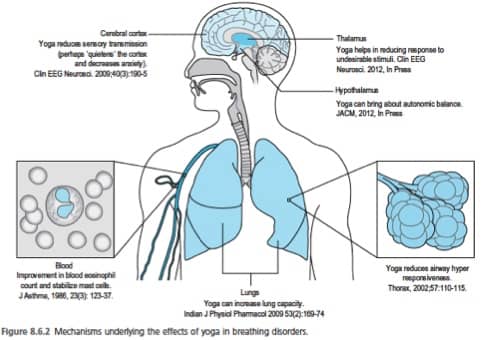
More recently evidence has emerged of the value, in some cases, of following a similar pattern (30 cycles 2x daily) but using ‘power breathing’ where inhalation is against resistance (Janssens et al 2015)


In this study:
- Individuals with nonspecific chronic low back pain (NSCLBP) have been shown to have suboptimal proprioceptive postural control (PPC) .
- NSCLBP is also strongly related to respiration and PPC is commonly impaired with compromised respiratory function.
- Individuals with NSCLBP have increased diaphragm fatiguability as well as decreased lumbar proprioceptive sensitivity.
- Breathing training used inspiratory resistance of 60% of maximal inspiratory pressure x 30 times, x 2 daily, for 8 weeks.
- Compared with the controls, the inspiratory muscle training group demonstrated better postural control; increased inspiratory muscle strength; decreased LBP
- Breathing retraining involved POWERbreathe Medic (HaB International Ltd., Warwickshire, UK), with the individual standing upright with the nose occluded
- Resistance was added with each breath generating negative pressure of 60% of Pimax (maximal mouth pressure)
- Participants performed 30 diaphragmatic breaths, 2 x daily, 7 days per week, for 8 weeks at a rate of 15 breaths per minute
- Results showed increased reliance on back proprioceptive signals, improved inspiratory muscle strength and reduced severity of LBP
Successful breathing rehabilitation involves the following key elements:
- Understanding the processes – a cognitive, intellectual awareness of the mechanisms and issues involved in BPDs and postural influences
- Retraining exercises & protocols, including aspects that operate subcortically, allowing replacement of currently habituated patterns with more appropriate ones
- Biomechanical structural modifications that remove obstacles to desirable and necessary functional changes
- Time for these elements to merge and become incorporated into moment-to-moment use patterns

Read about this book at:
http://astore.amazon.co.uk/leonchaitow-21/detail/0702049808
http://astore.amazon.com/leonchaitowco-20/detail/0702049808
REFERENCES
- Clifton-Smith T 2011 Breathing pattern disorders and physiotherapy: inspiration for our profession. Phys Ther Rev 16:75-86
- Hodges P et al . 2000 J Physiol. 522(Pt 1):165-175
- Hruska R. 1997 Influences of dysfunctional respiratory mechanics on orofacial pain. Dent Clin North Am. 41(2):211-227
- Janssens L et al (2015) Inspiratory Muscle Training Affects Proprioceptive Use and Low Back Pain.
Medicine & Science in Sports & Exercise. 47(1):12-19Kapreli E 2009 et al. Respiratory dysfunction in chronic neck pain patients. Cephalalgia. 29(7):701-710 - Lewit K. Relationship of faulty respiration to posture, with clinical implications. J Am Osteopath Assoc. 79(8):525-528
- McGill S et al.1995 Ergonomics. 38:1772-1792
- McLaughlin L et al 2011 Breathing evaluation and retraining. Man Ther 16:51-52
- Roussel N et al 2007. Low back pain: Climetric properties of the Tredelenburg test. J Manipulative Physiol Ther. 30(4):270-278
