In this post I have gathered a few reminders about Muscle Energy Technique (MET), when applied to joint restrictions in general, and the shoulder joint in particular…
In doing so I have leaned heavily on ‘words of wisdom’ from pioneer osteopaths……
….Also in this post – for those unaware of his influence on MET) – I wish to introduce one aspect of the work of Thomas Jefferson Ruddy DO….. a student of AT Still, who developed a unique and highly efficient approach that was absorbed into early MET methodology, in treatment of somatic dysfunction, that has largely been forgotten ….which he called Rapid Resistive Duction….and which I have renamed ‘Pulsed MET’
What might be causing joint motion restriction that is being treated?
‘[Irrespective of the cause]….treating a joint motion restriction as if the cause were tight muscle(s) is one approach that makes possible restoration of normal joint motion. Regardless of the cause of restriction, MET treatment, based on a ‘short muscle’ paradigm, is usually completely effective in eliminating blockage, and restoring normal range of motion, even when the blockage is due to non-muscular factors.’ (Mitchell Jr. 1998)
What forms the barrier of restriction?
‘As the [restriction] barrier is engaged, increasing amounts of force are necessary and the distance decreases. The term barrier may be misleading if it is interpreted as a wall or rigid obstacle to be overcome with a push. As the joint reaches the barrier, restraints in the form of tight muscles and fascia serve to inhibit further motion. We are pulling against restraints rather than pushing against some anatomic structure.’ (Kappler & Jones 2003)
Whose force should be employed in MET?
‘The therapist’s force is always the counterforce. A common mistake is to ask the patient to “resist my effort”. This ignores the factor of intentionality that ensures that core muscles are re-educated and rehabilitated. What works best is to tell the patient the exact direction of the action, the amount of force, and when to stop.’ (Mitchell Jr. 2009)
In what direction(s) should forces be directed during the post-contraction phase of MET, in treatment of joint restrictions?
Originally (1940s) MET was taught with joints being taken to their end of range (restriction) in three planes – for example flexion, side-flexion, rotation. MET applied in this way was often ‘very difficult, if not impossible.’ However, Lewit demonstrated that because segmental vertebral motions are coupled, if normal ROM can be restored in the coronal plane, normal motion will be restored in the other planes. Clinical experience suggests that MET procedures applied, using side-flexion (or translation), will usually release restrictions in other planes.’ (Mitchell Jr. 2009)
How long should an isometric contraction be maintained in MET treatment of joints?
‘The sensory(spinal) adaptive response in the … proprioceptor mechanism … probably takes no more than one tenth of second. Once that (sensory) adaptive response occurs, passive mobilization, during the post-isometric phase, can usually be accomplished without effort. … For joints, more than two seconds of isometric contraction is a waste of energy.’ (Mitchell Jr. 2009)
How strong should isometric contractions be in MET treatment of joints?
‘Strong or moderate force contractions – as initially used in MET – recruited too many of the ‘wrong’ motor units, and results were less that were hoped for. It was Lewit who drastically reduced the force generated by muscle contractions.’ (Mitchell Jr. 2009)
MET sequence:
‘There are six steps used in muscle energy treatment and they are repeated twice. 1) The area is positioned to engage the restrictive barrier. 2) The patient is instructed to contract the involved muscles with a specific intensity and in a specific direction (move the area in a specific direction). 3) The patient’s contraction is met with the appropriate counterforce (isometric, isotonic, isolytic) for 3–5 seconds. 4) The patient is instructed to slowly relax, and the physician relaxes the counterforce. 5) There is a pause to allow for muscle relaxation. 6) The area is repositioned to the new restrictive barrier and the sequence is repeated.’ (Carreiro 2009)
Title of Ruddy’s 1962 article
Ruddy’s description of Rapid Resistive Duction (known in this text as ‘pulsed MET’):
‘Resistive duction is a rapid succession of rhythmic muscle contractions against resistance by the [practitioner] for the purpose of establishing normal muscle tone, removing fascial tension and fixation, permitting freedom to tissue and body fluids.’ (Ruddy 1962)
RUDDY’S DESCRIPTION OF HIS METHOD
“The technic of employment of rapid rhythmic resistive muscle contraction is simple:
1. Resist the levers to which the correcting muscle is attached.
2. Patient contracts the muscle repeatedly, synchronous with the pulse rate and faster to double the pulse rate or higher, counting one-two, two-two, three-two, up to ten-two, the frequency at the close to be five-two in five seconds, if not an acute painful movement.
3. Press the part to be moved aiding the contracting muscle.
4. Counter pressure on the part articulating with the restricted unit.
5. Employ skeletal muscle contraction to pump visceral circulation.”
“The purpose of rapid rhythmic resistive duction is;
A) to increase the speed and strength of blood and tissue fluid flow, in skeletal, visceral and nerve structure insuring nutrient substances to each cell, and the removal of extrinsic toxins and wastes from the tissues
B) to create an homeostasis between the fasiculi of all muscles by correcting fixations, and reconditioning through muscle contraction
C) to engender normal afferent impulses to all nerve centres particularly the pre-motor cortical area for reestablishing normal tone.”
Illustration from Ruddy’s 1962 paper
Within that approach Ruddy famously cautioned that there should be:
‘No wobble; no bounce’
– emphasising the need for a rhythmic series of controlled contractions
Summary of MET use in joint treatment
- When treating complex joints, where there are numerous muscle attachments (e.g. pelvis, neck) clinical experience – and logic – suggests that before specifically focusing on the restricted joint, all major attaching muscles should receive MET attention in order to reduce hypertonicity.
- Treatment commences at the restriction barrier for all acute soft tissue conditions, and for all joint MET.
- For a joint, following a light isometric contraction (of agonist, antagonist, or other muscle(s) – depending on chosen direction of effort) – or the use of pulsed MET, tissues are taken to the new barrier, without force or stretching. One or two repetitions, using alternative directions of force application if the initial one was unsuccessful, are commonly recommended.
- Complex joint restrictions, for example involving a spinal segment, may be treated by attention to single directions of restriction, e.g. flexion or extension, or by taking the joint to its easy end-of-range in, for example, flexion, side-flexion and rotation – and then using a quite different direction for the pulsed or sustained contraction, for example translation.
- No stretch is ever used with joint mobilisation, when using MET.
- When using pulsed MET, the initial rhythmic resisted pulsation is usually towards the barrier. After approximately 20 rhythmic contractions, the muscle or joint is positioned at the new barrier. This process is repeated until there is no more gain – frequently using different directions of isometric effort.
- Visual and/or respiratory synkinesis may be useful, particularly in acute settings.
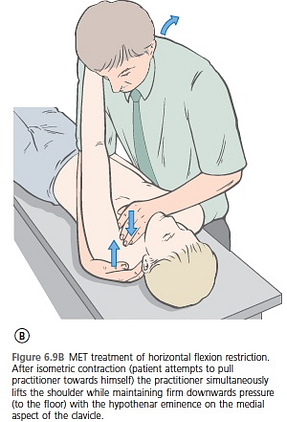
An example is illustrated here – showing treatment of the sternoclavicular joint (horizontal motion restriction), where MET can be usefully employed involving brief (3 to 5 seconds) isometric contractions, in almost any direction, to produce mobilising forces….or pulsed MET could be used instead.
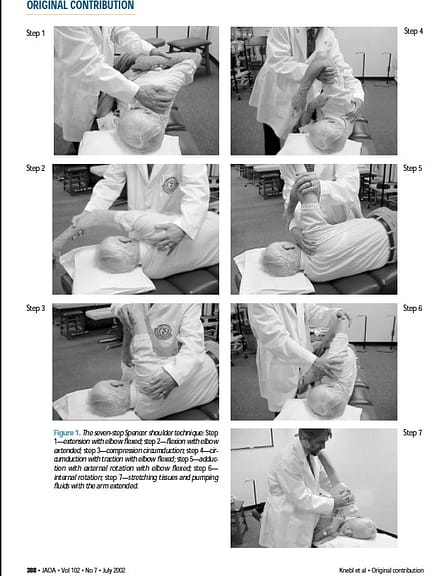
Spencer shoulder sequence incorporating MET
The Spencer shoulder treatment is a traditional osteopathic procedure (Spencer 1976, Patriquin 1992) that has in recent years been modified by the addition to its mobilisation procedures (described below) of MET. Clinical research has validated application of the Spencer sequence in a study involving elderly patients (Knebl 2002).
- In a study 29 elderly patients with pre-existing shoulder problems were randomly assigned to a treatment (Spencer sequence osteopathic treatment) or a control group.
- The histories of those in the two groups were virtually identical: approximately 76% had a history of arthritis, 21% bursitis, 21% neurological disorders, 10% healed fractures.
- 63% had reduced shoulder ROM as their chief complaint, and 33% pain (4% had both reduced ROM and pain).
- Treatment of the control (placebo) group involved the patients being placed in the same seven positions (see descriptions and Figs 6.5A–F) as those receiving the active treatment; however, the one element that was not used in the control group was MET (described as the ‘corrective force’) as part of the protocol. Home exercises were also prescribed.
- Over the course of 14 weeks there were a total of eight 30-minute treatment sessions. Functional, pain and ROM assessments were conducted during alternate weeks, as well as 5 weeks after the end of treatment.
- Over the course of the study both groups demonstrated significantly increased ROM and a decrease in perceived pain. However after treatment:
‘Those subjects who had received osteopathic manipulative treatment [i.e. muscle-energy-enhanced Spencer sequence] demonstrated continued improvement in ROM, while the ROM of the placebo group decreased.’
The researchers concluded: ‘Clinicians may wish to consider OMT [i.e. Muscle Energy Technique combined with Spencer sequence] as a modality for elderly patients with restricted ROM in the shoulder.
Illustration from Kneble 2002 showing Spencer Sequence
- A firm controlling hand stabilises the scapula and clavicle to the thorax, so that ALL motion occurs in the glenoid fossa
- Various directions of motion are tested and wherever a restriction is noted MET is employed, after which movement continues to a new barrier (FIRST SIGN OF RESISTANCE)…no stretching is ever used in joint MET
NOTE:
In any of the Spencer sequence positions treatment of identified restrictions may involve isometric contractions towards, or away from, the barrier, or in any other direction that results in an increased range of movement.
Alternatively, pulsed MET may be employed.
Illustrations from of spencer Sequence (Muscle Energy Techniques 4th edition, Chaitow 2013)
It is suggested that instead of, or in addition to, regular MET, Pulsed MET may offer better outcomes.
Previous posts that touch on similar themes include:
In 2011:
https://leonchaitow.com/…/pulsed-muscle-energy-technique-ru…/
In 2011:
https://leonchaitow.com/…/pulsed-muscle-energy-technique-me…/
In 2012:
https://leonchaitow.com/…/21/update-on-muscle-energy-techni…/
In 2012:
https://leonchaitow.com/…/barriers-met-feather-edge-or-stre…/
MET BOOK:
UK & Europe
http://astore.amazon.co.uk/leonchaitow-21detail/0702046531
USA
http://astore.amazon.com/leonchaitowco-20/detail/0702046531
REFERENCES
- Carreiro, J., 2009. Pediatric Manual Medicine (First edition). An Osteopathic Approach, p. 155–192.
- Kappler, R.E., Jones, J.M., 2003. Thrust (High-Velocity/Low-Amplitude) techniques. In: Ward, R.C. (Ed.), Foundations for osteopathic medicine, second ed. Lippincott, Williams & Wilkins, Philadelphia, pp. 852–880.
- Knebl, J.A., Shores, J.H., Gamber, R.G., et al., 2002. Improving functional ability in the elderly via the Spencer technique, an osteopathic manipulative treatment: A randomized, controlled trial. Journal of the American Osteopathic Association 102 (7), 387–396.
- Mitchell, F. Jr., 2009. Interview. In: Franke, H. (Ed.), The History of MET In: Muscle Energy Technique History-Model-Research. Verband der Osteopathen Deutschland, Wiesbaden.
- Mitchell F., Jr., 1998. Muscle Energy Manual, Vol. 2. MET Press, East Lansing, p. 1.
- Patriquin, D., 1992. Evolution of osteopathic manipulative technique: the Spencer technique. Journal of the American Osteopathic Association 92, 1134–1146.
- Ruddy, T.J., 1962. Osteopathic rhythmic resistive technic. Academy of Applied Osteopathy Yearbook, 1962, pp. 23–31.
- Spencer, H., 1976. Shoulder technique. Journal of the American Osteopathic Association 15, 2118–2220.